Are NHS waiting times improving?
Are NHS waiting times improving? Recent numbers show mixed results. In December 2024, 58.9% of patients waited less than 18 weeks. This is a small improvement but far below the 92% goal. Over 200,000 patients still wait more than a year. Thousands also face delays longer than 65 weeks. These numbers indicate ongoing problems.
Long waits can affect you as a patient. Delays might exacerbate serious illnesses. They can also cause stress and diminish trust in care. For the NHS, these delays consume resources and incur additional costs. This impacts other services such as A&E and ambulance response times.
Key Takeaways
NHS waiting times are mixed. Only 58.9% of patients wait less than 18 weeks. This is much lower than the 92% goal.
Long waits can make health problems worse. They also cause more stress for patients. Quick care is very important.
Not enough money and staff are big reasons for long waits in the NHS.
Technology like smart tools and online doctor visits helps make things faster. It also cuts down waiting times.
To fix this long-term, the NHS needs better funding, more staff, and a focus on stopping illnesses early. This will help healthcare last longer.
Are NHS waiting times improving?
Latest statistics and trends
Are NHS waiting times really getting better? The latest data shows mixed results. During the pandemic, patient numbers waiting for treatment grew a lot. They increased from 450,000 to 775,000 by late 2023-24. The average wait for treatment also reached over 29 weeks. While there has been some improvement, waits are still twice as long as before the pandemic.
Hospitals are trying new ways to fix this issue. They use tools like predictive analytics and real-time tracking. These help them plan better and use resources wisely. By working more efficiently, they hope to cut waiting times. But the problem is so big that progress is slow.
Improvements since the pandemic
Some improvements have been seen since the pandemic. For example, the number of patients treated within four hours rose slightly. It went from 70.8% in 2022/23 to 72.1% in 2023/24. This is a small but good sign. However, more patients waited over 12 hours in A&E, with an increase of 29,319. This shows there are still big challenges.
These changes show that focused efforts can help. Hospitals are using technology to make their work smoother. While these steps are helpful, they are not enough to meet the rising demand for NHS services.
Areas where waiting times remain a challenge
Even with some progress, waiting times are still a big problem in some places. For example, 29% of patients in Wales and 25% in Scotland are still waiting for care. In England, the number is lower at 21%. This shows that resources are not shared equally, and local solutions are needed.
Planned treatments also face long delays. In February 2020, 1,600 patients waited over a year for care. By March 2022, this number grew to over 300,000. Fixing these delays needs more money, better planning, and creative ideas.
Factors affecting NHS waiting times
Money and resources
Money is key to how fast you get NHS care. When there isn’t enough money, hospitals can’t keep up. For example, they may not buy needed tools or expand buildings. This slows down waiting times, especially for planned surgeries.
How money is shared also matters. If it’s not given based on patient needs, some places wait longer. Rural areas often have bigger problems because they have fewer hospitals. Fixing this needs better planning and smart spending.
Not enough staff
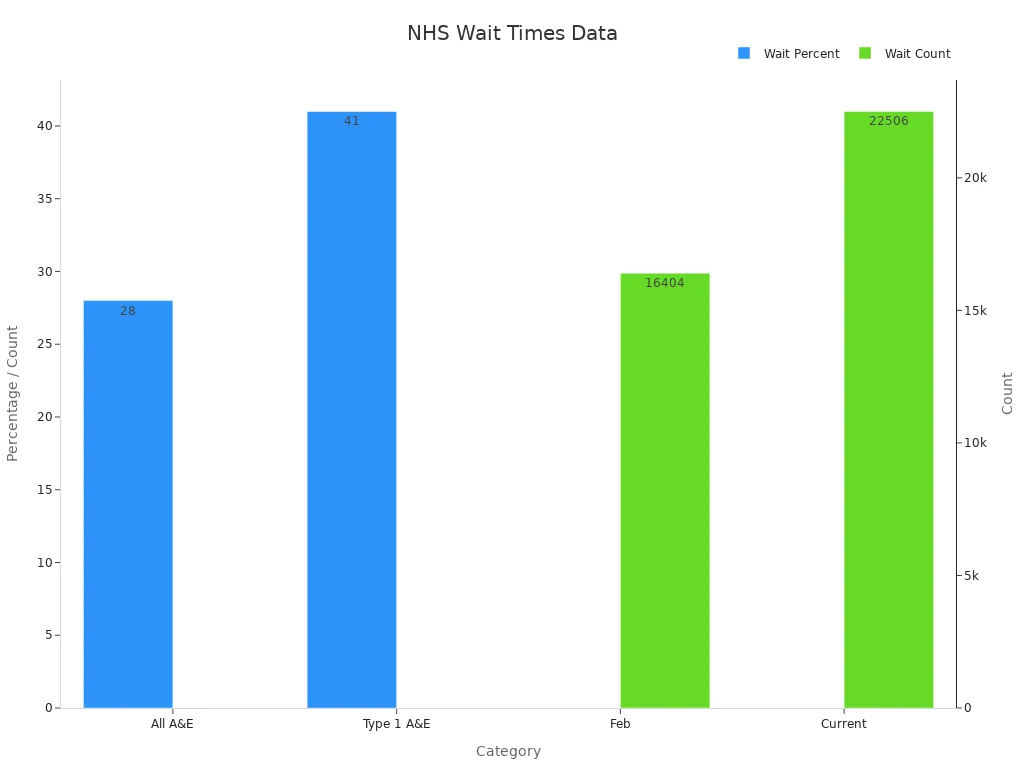
The NHS doesn’t have enough doctors, nurses, or other workers. This means fewer patients get treated quickly. A&E departments feel this problem the most. The table below shows how bad it is:
Metric | Value |
|---|---|
People waiting over 4 hours (all A&Es) | |
People waiting over 4 hours (type 1 A&Es) | 41% |
Total A&E visits in March | 2.1 million |
Rise in A&E visits since March 2021 | 28.5% |
People waiting over 12 hours | 22,506 |
People waiting over 12 hours (February) | 16,404 |
Hiring new staff is slow and training takes time. Even when new workers join, it doesn’t fix the problem right away.
More patients and system struggles
The NHS is busier than ever, which adds pressure. Events like Covid-19 made more people need care. This means longer waits in all areas.
Problems in one part of the NHS affect others. For example, slow ambulance times make A&E too crowded. This chain reaction makes it harder to shorten waits. The chart below shows how these issues connect:
To fix this, we need many solutions. It’s not just about demand but also making the system work better.
Impact of NHS waiting times

Effects on patient health and outcomes
Long waits can seriously affect your health. Delays in care often make illnesses worse. This is especially true for less urgent cases. Longer waits have been linked to more deaths. For example:
People with long-term illnesses may get worse without quick care.
Those needing surgery might feel more pain or lose movement.
Waiting longer can also harm your mental health. Stress and worry often grow while waiting for treatment. This can hurt your overall happiness and well-being.
Strain on NHS staff and resources
Long waits put a lot of pressure on NHS workers. More patients mean staff have to work harder than ever. This can make them feel tired and unhappy at work.
Here are some important facts:
By March 2022, over 300,000 people waited over a year for care. In February 2020, only 1,600 people waited this long.
A&E departments often don’t have enough staff, causing delays.
During winter 2022/23 and 2023/24, 10% of emergency admissions were delayed.
The number of people waiting over 12 hours in A&E rose from 410,092 in 2022/23 to 439,411 in 2023/24. This shows there aren’t enough hospital beds or resources. These delays make it harder for staff and lower the quality of care you get.
Public trust and perception of the NHS
When waits get longer, people trust the NHS less. Delays can make you doubt if the system works well. This can lead to frustration and unhappiness with the care provided.
People often ask, "Are NHS waiting times improving?" Some progress has been made, but big problems remain. To rebuild trust, the NHS needs to show clear improvements in wait times and care quality.
Actions to address NHS waiting times
Government initiatives and funding
The government is taking steps to reduce NHS waiting times. One main action is giving more money to the NHS. For example, the budget has grown to help with the backlog. Still, 7.5 million people in England are waiting for hospital care. Over 3 million have waited longer than the 18-week goal, which hasn’t been met since 2016.
To fix this, the government promises more resources to increase capacity. This includes building new hospitals and improving old ones. But the problem is still very big. For example, over 50,000 patients have waited for hospital beds in recent years. These numbers show that more money and better planning are needed.
Evidence Type | Statistic/Detail |
|---|---|
Total waiting list | 7.5 million people in England awaiting hospital treatment. |
Maximum waiting time target | 18 weeks (not met since 2016). |
Patients waiting longer than 18 weeks | Over 3 million. |
Hospital treatment waiting list growth | Nearly 5 million by 2020, surged to 7.5 million by 2023. |
Strategies to improve staffing levels
Not enough staff is a big problem for the NHS. Long waits in A&E or for surgeries often happen because there aren’t enough doctors or nurses. The government is trying to hire more healthcare workers. Training programmes have also been made bigger to prepare new staff.
But hiring and training take time. For now, the NHS uses temporary workers and hires from other countries. These help for a while but can’t solve the problem long-term. To keep staff, better pay and working conditions are needed. Reducing stress and making jobs more enjoyable are also important.
Role of technology and innovation
Technology helps make NHS waiting times shorter. Hospitals now use digital tools to work faster. For example, predictive analytics shows when patient numbers will rise. Real-time tracking helps use resources better.
Telemedicine is also growing, letting you talk to doctors online. This reduces pressure on hospitals and speeds up care. Tools like AI can find illnesses faster, making care more efficient. These ideas are helpful but need money and training to work well.
Tip: Using technology not only saves time but also makes care better.
Long-term solutions for sustainable healthcare
To make the NHS sustainable, we need long-term plans. These plans should fix the main reasons for long waiting times. The system must handle more patients while still giving good care. Below are some important ways to improve things.
Adding more hospital beds is very important. The Health Foundation’s REAL Centre says the NHS will need 23,000–39,000 extra beds by 2030/31. This is to keep care levels the same as in 2018/19. More beds mean more patients can get treated on time. This will ease the pressure on current hospitals.
Technology is key to improving healthcare. Tools like predictive analytics help hospitals plan better. They can predict patient numbers, staff needs, and resources. Using this information wisely stops delays and improves care.
Planning for staff is also crucial. Hiring and keeping healthcare workers must be a top focus. Better pay, good working conditions, and career growth can attract skilled staff. A happy workforce can manage the growing number of patients better.
Preventing illnesses is another way to reduce NHS demand. Promoting healthy habits and early treatment stops problems from getting worse. This helps patients stay healthier and reduces the load on hospitals.
A strong NHS needs all these ideas together. By improving capacity, using technology, supporting staff, and focusing on prevention, we can build a system that works well now and in the future.
Note: Planning ahead isn’t just about fixing today’s issues. It’s about creating a system ready for future challenges.
Are NHS waiting times getting better? The numbers show mixed results. Many patients still face long waits for treatment. Not enough staff and linked NHS services make it tough to hit goals. These problems harm patient health, stress workers, and lower public trust.
There is some progress, like using technology and more government money. But lasting changes need smarter resource use and more workers. Efforts should also focus on making healthcare fair for all. Fixing these problems can help the NHS handle more patients and give better care to everyone.
FAQ
Why are NHS waiting times so long?
NHS waiting times are long because more people need care. There aren’t enough staff or resources to meet the demand. The pandemic made things worse by adding more patients to the list. Problems in how resources are shared also cause delays.
Why does the NHS find it hard to hire more staff?
The NHS struggles to hire because pay is low and stress is high. Working conditions are tough, and many workers leave due to burnout. Training new staff takes a long time. Hiring from other countries helps but doesn’t fix the problem forever.
Why is technology useful for cutting waiting times?
Technology makes the NHS work faster and better. Tools like predictive analytics help hospitals plan ahead. Telemedicine lets patients see doctors online, reducing pressure on hospitals. These changes save time and improve care.
Why do some areas have longer waiting times than others?
Some areas wait longer because resources aren’t shared equally. Rural places often have fewer hospitals and staff, causing delays. Cities may have too many patients, which also leads to longer waits.
Why hasn’t the NHS reached its 18-week target?
The NHS hasn’t met the 18-week goal since 2016. This is because more people need care, and there aren’t enough staff or space. The pandemic made the backlog worse, and funding problems add to the challenge.
See Also
Exploring Recent Developments in NHS Waiting Times for Seniors
How NHS Waiting Times Impact Patient Health and Happiness
Steps Patients Can Take to Shorten NHS Waiting Times
Understanding Why NHS Waiting Times Seem Endless Today
Evaluating NHS Waiting Times Under Labour and Conservative Leadership

